Recovery is in Danger

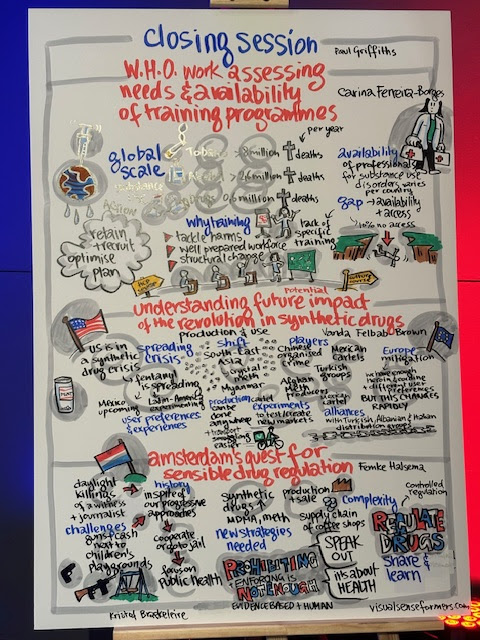
We just returned from an amazing trip to Portugal where we presented at the international Lisbon Addictions Conference. There were 2,231 people from 103 countries. Truly remarkable!
We had the opportunity to visit a mobile methadone program, Ares do Pinhal, a Social Solidarity Institute established in 1986. They began with therapeutic communities in order to support individuals with substance challenges (largely heroin and alcohol). In the 90’s they expanded into Harm Reduction services as 1% of the population in Portugal was addicted to heroin at the time. Dr Joao Golao, along with a group of other healthcare professionals and advocates, designed the drug decriminalization policies that birthed the mobile methadone program in 2001 as part of the response. Today, there are two mobile units that serve over 1,300 individuals across 5 sites on a daily basis!

Being around the bus was amazing as people went about their business like nothing. No onlookers, no people hanging out in the streets. It was as simple as getting an ice cream cone at the ice cream truck. People go up to the window, give them their assigned number and in turn are handed their medication which they can take as they wish. They don’t have to be monitored to take their medication. People were very friendly, many of them saying hello to others and a few even jumped into pictures with our group! This was a tell tale sign of how they are treated there. Like humans. Drug addiction is looked at as a public health issue, not a moral one to be punished. “At the end of the day, drug use is a basic human right,” said one of the social workers.
Across the city, their first formal Drug Consumption Room (DCR) opened 20 years after decriminalization. Over 120 people per day come to use pre-obtained substances via smoking or injection, mainly crack cocaine and heroin while being supervised. Here, they have access to Sterile consumption equipment including new needles, glass pipes, foil and at times, drug testing equipment as well. If they’d like, they can see a primary care physician, a nurse or a psychologist. Individuals can be transported to other medical services while having the support of a social worker, peer educators as well as the community. Hugo Faria, the Psychologist who is the director shared with our group that there have been under 10 overdoses there in the past year, none of them fatal. In the past few years, Portugal has averaged 80 overdose deaths per year.


The Lisbon Addictions Conference had over 600 presentations. Many of them, science based presentations made by PhD students and statistics from professionals working in the field. One thing that we noticed was that there wasn’t a lot of talk or presentations on peers. After speaking with people from across the globe, New Zealand to South Africa, Palestine to Ireland to British Columbia, we noticed that the majority of peers are working in Harm Reduction. There were under ten presentations on peers or the peer workforce. Our group having 3 of them. As we were writing on a board prompting people for recommendations for the next conference, adding Recovery Capital and Recovery Oriented Systems to the list, one of the people from EUDA (European Union Drugs Agency) commented. “We don’t use this language (recovery) here. For a second I had no words and then asked her if she can explain. “The United States presents it as abstinence and it is not part of our philosophy here,” she said. “We know that people use drugs and most of them have many different goals that don’t involve abstinence. We are here to help people be well, not to tell them what to do.” We immediately agreed with her and discussed it together.

Unfortunately, she is right. We have a great definition from SAMHSA which supports the Infinite Pathways and yet, programs are largely focused on abstinence based compliance. There is an agenda for people based on morality, fear and the need for control. Society continues to punish drug users, often discriminating against them with a beer in hand and policies are designed specifically to support this. Does that sound like we’re “meeting people where they are at?” I know that many of us don’t have that outlook, nor approach. The thing is that the agencies and systems that we inhabit and work with do. These barriers are deliberate as they exist within treatment settings, impeding individuals in moving through the continuum of care. It is no surprise that less than 10% of the individuals in need of treatment actually get it and 30 days after people are discharged from treatment, only 25% of them are still engaged with some kind of support. So what’s happening with the other 90% of the people not showing up or the 75% no longer getting support? That’s right, their challenges continue to impact them as well as their communities in so many ways while many of them multiply.
This leaves us with great discrimination along with an abyss in our continuum of care. Our language continues to mimic the dominant narrative and our approach is shutting the door on people, who might be seeking help and instead are being told they have to fit into the mold in order to belong or be cast aside.
Recovery is in Danger. Most people don’t identify with it. Our language, our approach, our methods, our standards and our policies must be looked at. When is this going to change and what do you want to do about it so that people are called in as opposed to being called and pushed out?
It’s more crucial than ever to maintain the fidelity of the recovery model and support the individual in identifying whatever it is that they want for themselves, regardless of what they call it or not. That deserves some dignity, because it’s not our recovery or wellness, it’s theirs.
At CHOiCE Recovery Coaching, we are here to support the needs and wants of individuals as THEY see fit as we educate ourselves, learning with the communities around us.
FREE Training Grant
Have thoughts, comments, questions or concerns? We would LOVE to hear from you! recovery@
Thank YOU for Championing Recovery!